By Lauren Colton, Leila Matta, and Colleen Tapen
The renewal of Medicaid coverage following the end of the Public Health Emergency in 2023 has posed significant challenges for millions of Americans. More than 20 million people have been automatically removed from Medicaid since May 2024, and government teams are grappling with ensuring eligible individuals can renew their coverage and continue receiving essential health benefits.
As governments across the country focused on how to increase “ex parte” (i.e. automated) renewal rates, U.S. Digital Response (USDR) wanted to understand how people are experiencing the renewal journey when their coverage cannot be renewed automatically. Equipped with a deep understanding of these families’ experiences, we hope to help state and local governments identify and replicate what’s working, and focus on opportunities for improvement.
In our full report, released today, we share the experiences of 18 families who have had to navigate the Medicaid renewal journey for themselves or family members. We explore each phase of this journey in-depth to highlight what’s working well and suggest opportunities for improvement. We hope to inform government, nonprofit, and public sector teams seeking to improve the experience of renewing Medicaid and other benefits anywhere in the United States.
The problem
The end of the official Public Health Emergency in 2023 marked a critical juncture for Medicaid recipients. The continuous coverage requirement that was put in place due to the COVID-19 pandemic was lifted, causing millions of individuals on Medicaid to need their coverage renewed. While many governments across the country worked tirelessly to implement “ex-parte” (or automatic) renewals, millions of Americans still needed to go through a manual renewal process, some for the first time. The abrupt shift led to widespread immediate disenrollment, affecting millions of Americans who depend on Medicaid for their healthcare needs. Government teams across the country are working to navigate the complexities of the renewal process, and many are working to prevent even more eligible individuals from losing their coverage.
This shift has deep impacts on families who need to navigate renewing for themselves, their children, or others they care for. While the process varies from state-to-state, there are clear commonalities that the families we talked to went through, and aspects where the system worked, and where it did not.
The journey of residents renewing Medicaid
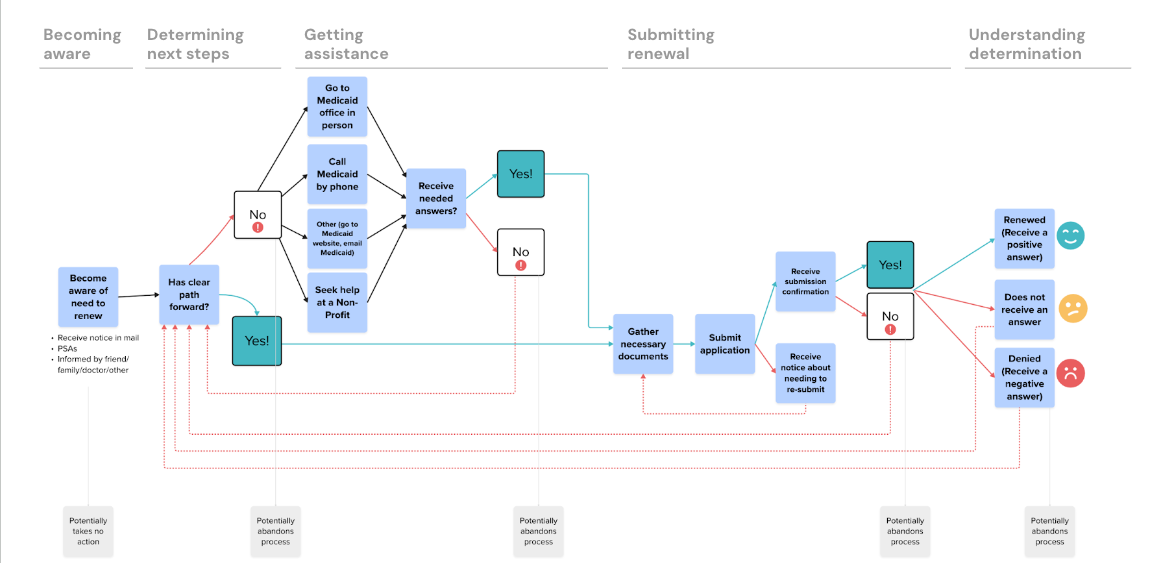
By listening to people’s stories and conducting in-depth interviews with real families going through the renewal process, our team was able to capture insights not always evident in existing research and news reports. Residents described the Medicaid renewal journey as frequently non-linear and complex, with multiple hold-up and drop-off points, as depicted below.
Meet some of the residents we spoke to, and see the report for more robust depictions of their experiences:
Ashley: a single mother who had multiple Medicaid office visits about renewing, was confused by documentation requirements, experienced prolonged anxiety, and lost trust in the online portal.
I emailed and they never got back. So I sat on the phone for 2 hrs. Why say 12 to 48 hr email response if you don’t bother to even respond. There’s no service there. It made me feel unheard, not cared about. It makes you feel not worthy.
Kendra: a working parent and caregiver to an elderly parent on the Medicaid Waiver program, who faced stress over timelines and the potential loss of coverage for her mom, after five years of work to receive the coverage.
Our support planner gave us my mom’s previous application and walked us through the process: The packet is going to come next month, and here are the documents you need… So I feel pretty good about what is needed to renew my mom.
Joe & Kathy: a couple with four children on Medicaid, who struggled to understand notices and received help from a community organization to navigate the process.
At times the app says we’re denied, but we call — ‘No, you’re not denied. It’s all great. You have everything turned in.’ It is tough to do a 1.5 hr call to find the truth. We’re panicking, scared. My kid has a shunt, and any moment he could need emergency surgery. So we freak out when it says denied.
The following journey map visualizes the overarching process that individuals undergo, highlighting key stages and challenges:

In our full report, we open up each of these stages, sharing insights, recommendations, and concrete examples of what’s working, and how states can support applicants throughout their journey.
Key opportunities
Based on conversations with residents, there are several key factors that could make the renewal process easier to navigate. The top areas of focus for states and counties to improve the renewal process include proactive communication, enhanced customer support, and providing clarity on status.
Key opportunity 1: Head off questions and confusion from the start
- Clear initial communication: Explain what residents should expect and what to do next right from the start.
- Increase digital communication: Send texts and emails to decrease communication gaps, to avoid issues with unreliable mail like address changes and to provide more timely updates.
“I never got emails from them, which was insane. I checked all my emails and even my junk. Because my mom throws out my mail, sometimes I don’t get updates.” — Research participant
Key opportunity 2: Enhance Customer Support to Resolve Uncertainty
- Streamline Issue Resolution: Help individuals resolve their issues without being transferred, referred to a caseworker, or required to call back.
- Respectful Assistance: Bolster respectful and dignified customer service to improve the overall experience, regardless of language.
“I felt like no one I talked to on the phone knew how to help, because multiple times they transferred me, even though I just talked to that department.” — Research participant
Key opportunity 3: Reduce Confusion Throughout the Process
- Provide End-to-End Status Tracking: Implement systems for end-to-end status tracking to reduce the need for additional calls and visits, and prevent contradictory updates that sometimes arise.
- Clarify Termination Reasons: Clearly explain termination reasons, such as children aging out, and provide guidance on next steps.
“My daughter was kicked off and I wanted to dispute it but I didn’t know how. When I turned in my renewal, I put a letter in there to dispute my daughter’s to try to help.” — Research participant
For a comprehensive list of opportunities and detailed recommendations, refer to the full report from USDR.
Overall, the stakes feel incredibly high for people renewing Medicaid. Many reported widespread uncertainty, with significant anxiety that undermines trust in the system. Despite these challenges, there were bright spots and areas where the process worked well.
Bright spots
1. Proactive Outreach: Some states implemented proactive outreach programs and ad campaigns, contacting individuals before their renewal dates to guide them through the process.
“You hear it on the radio: make sure you watch out for the renewal, and mail back the forms that you have to fill out.” — Research participant
2. Streamlined Online Renewals: In states with pre-populated renewals or well-designed and up-to-date online renewal portals, individuals found it easier to manage their renewals.
“Some information is prefilled. We are like, ‘Any changes? Nope.’ And we put submit. It is really quick.” — Research participant
The Medicaid renewal process presents significant challenges, but change is happening and is possible. Examples from various states demonstrate that with proactive measures, clear communication, and supportive services, the renewal experience and outcomes can be significantly improved. Taking small steps to streamline and humanize the renewal process can have a huge impact on the lived experience of those going through the process. We encourage states, advocates and others involved in the process to bring in the experience of those who have had to go through the renewal process to identify opportunities to bring change to your community.
